Health
Kiwi CEO Navigates Chaos of American Healthcare System
Brad Porter, the chief executive of Orion Health, recently faced a disorienting experience within the American healthcare system while on a family trip to California. Following a joyful visit to Disneyland, his nine-year-old son began struggling to breathe. With a flight back to New Zealand scheduled for later that evening, Porter found himself battling the very chaos he aims to address through his work in health technology.
His initial stop was a local pharmacy, where he encountered a stark contrast to the healthcare system in New Zealand. In his home country, pharmacists can assess minor illnesses and provide immediate care. Instead, in California, he was handed a box of Tylenol and told that no advice could be given due to liability issues. This experience highlighted a systemic flaw: qualified healthcare professionals restricted from assisting patients due to regulatory constraints.
Seeking urgent care, Porter was informed that pediatric patients were not seen at that facility, even in the case of a child experiencing significant wheezing. Fortunately, he spotted a children’s medical group nearby and, using his Kiwi accent, managed to secure an appointment that is typically reserved for insured patients.
Upon arrival, he was met with an iPad intake form that contained numerous fields, disclaimers, and consents. While the technology seemed modern, the physician assistant took notes on paper because their electronic medical record (EMR) system only allowed for one user at a time. Throughout the visit, three different clinicians provided compassionate care, yet each asked the same questions he had already answered on the iPad. This redundancy underscored the inefficiencies within the system.
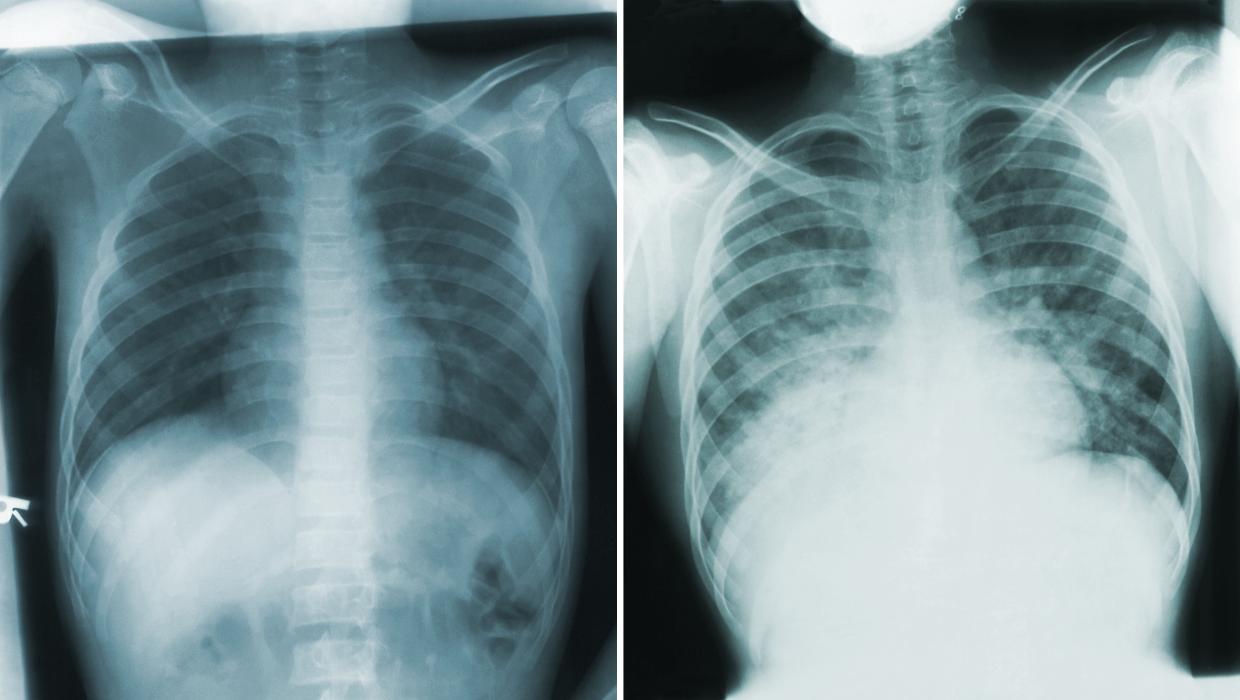
When the diagnosis of post-viral asthma was made, confusion continued. The physician prescribed albuterol, but Porter, familiar with the medication’s international name, recognized it as salbutamol. This moment revealed a deeper issue: healthcare systems often speak in different dialects, not only in medication names but also in data formats. Names such as EMR, Shared Care Record (SCR), and Health Information Exchange (HIE) contribute to the fragmentation of information.
Porter noted that a standard like the International Patient Summary (IPS) could serve as a universal language for health data, potentially allowing his son’s asthma plan to follow him back to New Zealand seamlessly. Despite the thoroughness and care of the clinicians, the experience left him feeling the complexities of navigating payment. He was presented with an itemized bill that suggested an expectation of negotiation, a practice that is foreign to many healthcare systems worldwide.
His observations led him to consider the paradox of American healthcare, which boasts world-leading innovations but often operates with outdated processes. Talented clinicians are hindered by disconnected software, with financial considerations sometimes prioritized over patient care.
Reflecting on his experience during the flight home, Porter contemplated the differences between New Zealand and the United States. While New Zealand is often perceived as smaller and simpler, it too lacks a true national shared care record. Patients frequently arrive at hospitals where their medical histories are unavailable, complicating care.
Porter’s brief exposure to the American system served as a reminder that while the chaos in the US is apparent, complacency exists in New Zealand’s system as well. He emphasized the urgent need for New Zealand to advance towards a comprehensive shared care record that tracks patients from birth through retirement. This initiative would connect pharmacists, general practitioners, and hospitals, allowing for a more cohesive healthcare experience.
Emphasizing the role of technology, Porter argued that without proper integration, the potential benefits of artificial intelligence (AI) cannot be fully realized. AI could streamline processes, translating terminology and summarizing patient histories. Had the systems been integrated, his son’s asthma pattern might have been recognized beforehand, potentially averting the day’s turmoil.
Ultimately, while his son recovered and they returned home safely, Porter’s experience left him acutely aware of the fragility of even the most advanced healthcare systems. He believes that New Zealand has a vital opportunity to learn from his experiences in the US, advocating for a connected, patient-centered healthcare model that prioritizes collaboration among healthcare professionals and systems.
-

 Sports2 months ago
Sports2 months agoNetball New Zealand Stands Down Dame Noeline Taurua for Series
-
 Entertainment2 months ago
Entertainment2 months agoTributes Pour In for Lachlan Rofe, Reality Star, Dead at 47
-

 Entertainment1 month ago
Entertainment1 month agoNew ‘Maverick’ Chaser Joins Beat the Chasers Season Finale
-

 Sports2 weeks ago
Sports2 weeks agoEli Katoa Rushed to Hospital After Sideline Incident During Match
-

 Sports2 months ago
Sports2 months agoSilver Ferns Legend Laura Langman Criticizes Team’s Attitude
-

 Politics1 month ago
Politics1 month agoNetball NZ Calls for Respect Amid Dame Taurua’s Standoff
-

 Entertainment3 months ago
Entertainment3 months agoKhloe Kardashian Embraces Innovative Stem Cell Therapy in Mexico
-

 Sports2 weeks ago
Sports2 weeks agoJamie Melham Triumphs Over Husband Ben in Melbourne Cup Victory
-

 World4 months ago
World4 months agoPolice Arrest Multiple Individuals During Funeral for Zain Taikato-Fox
-

 Sports3 months ago
Sports3 months agoGaël Monfils Set to Defend ASB Classic Title in January 2026
-

 Entertainment2 months ago
Entertainment2 months agoTyson Fury’s Daughter Venezuela Gets Engaged at Birthday Bash
-

 Sports2 months ago
Sports2 months agoHeather McMahan Steps Down as Ryder Cup Host After Controversy

















